To Buy Ivermectin Online Visit Our Pharmacy ↓
Ivermectin Controversies and Misinformation during Pandemics
How a Popular Off-label Drug Became Viral
Early stories of dramatic recoveries spread fast online, mixing hope and confusion; a few clinicians wrote informal Rx notes and social clips.
Content creators amplified anecdotes, not trials, turning scarcity and charismatic voices into viral momentum; journalism struggled to clearly parse science from spectacle.
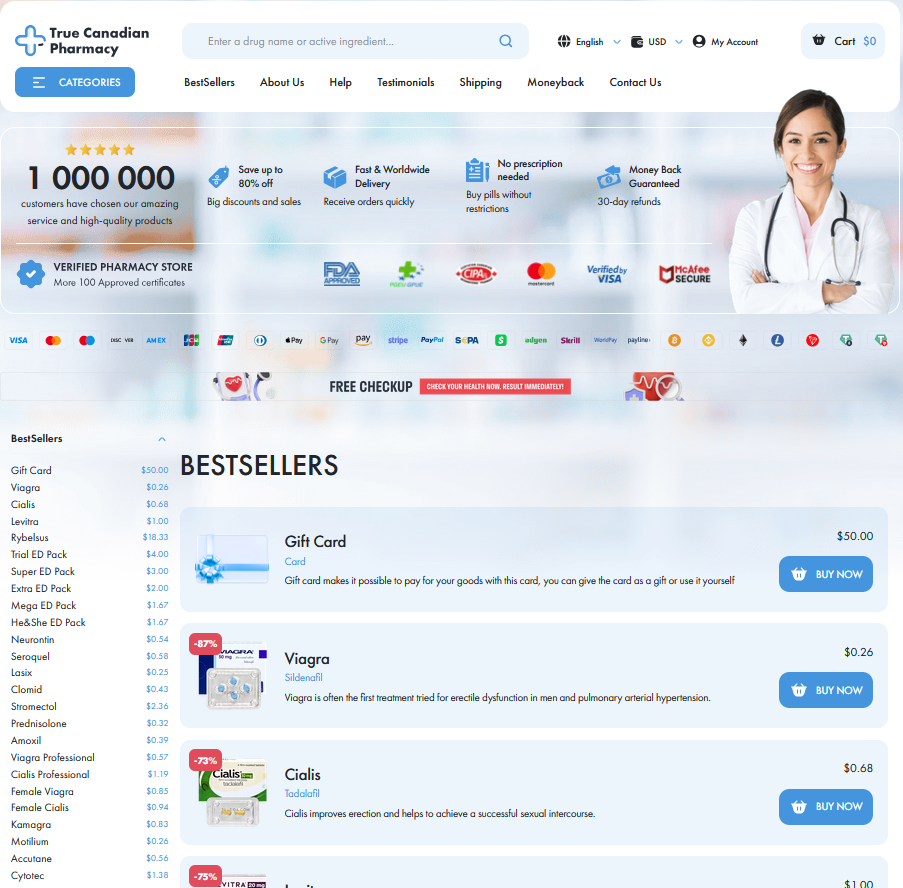
Pharmacy chains saw spikes, hoarding and off-label demand; regulators flagged risky prescriptions and issued warnings as some providers were labeled quack
Hype
The journey from hopeful remedy to cultural phenomenon shows how social proof, convenience and distrust can outpace careful trials and regulatory caution and consequences.
Science Versus Anecdotes: Interpreting Shaky Clinical Evidence
Early in a crisis, compelling personal stories often outrun formal trials. A single patient claim that ivermectin cured them travels faster than measured outcomes, and social feeds reward emotional narrative over nuanced data. This mismatch creates fertile ground for confirmation bias and cherry picking of favorable anecdotes.
Small, uncontrolled studies and preprints muddy interpretation: signals, not proofs, become headlines. Clinicians balance urgent care against the need for randomized evidence, while frustrated patients ask for an Rx or turn to OTC alternatives when guidance seems absent. Misinformation thrives where patients seek quick fixes, forming shadow markets and risky self-medication patterns.
Journalists and clinicians should explain uncertainty clearly, emphasizing effect sizes, confidence intervals, and harms. Rooting public messages in transparent methodology and avoiding sensational anecdotes reduces harm and builds trust. Clear, empathetic communication can reduce the allure of miracle claims, saving lives.
Media, Influencers, and the Amplification of Falsehoods
News cycles fast-forwarded a hopeful story into a global sensation: a cheap antiparasitic, ivermectin, touted as a miracle by vloggers and pundits. Clicks and outrage outran cautious science, and headlines preferred certainty over nuance.
Short clips simplified complex studies, cherry-picking case anecdotes that spread as if peer-reviewed. Algorithms rewarded engagement, not accuracy, so rumors amplified while retractions struggled to keep up.
Influential personalities with followings framed treatments, urging followers to demand Script or stock up at pharmacies, bypassing medical advice and fueling off-label use and black-market demand.
Public health communicators must counter false narratives with clear data, timely corrections, and trusted voices to rebuild confidence and steer people away from quacks and unsafe OTC substitutions.
Health Systems, Regulators, and Mixed Messaging Fallout
Hospitals scrambled as shifting advisories left clinicians uncertain; patients demanded unproven remedies like ivermectin while supply chains strained and pharmacists faced ethical triage decisions often at the counter.
Regulators oscillated, issuing rapidly changing guidance; insurers and hospitals adjusted the Formulary - List of covered medications, creating confusion about access, coverage, and appropriate prescribing for clinicians and patients.
Frontline doctors received mixed signals, watched social media anecdotes outrun data, and fielded demands for off-label Rx - Prescription fills that conflicted with evolving protocols and stewardship goals daily.
Trust eroded as patients doubted official advice; clinics rerouted scarce supplies, some resorted to pragmatic substitutions, while communication reforms were urgent to restore confidence and rebuild systems across regions.
Real-world Harms: Shortages, Poisoning, and Missed Treatments
Misinformation drove desperate demand for ivermectin, emptying shelves and disrupting supply chains. Pharmacies reported short fills and frustrated patients; clinicians struggled to replace off-label orders with evidence-based treatments. Tales of self-medication and poisoning surfaced.
Hospitals saw missed windows for timely antivirals, and poison control centers fielded calls about livestock formulations and inappropriate dosing.
Harm
Impact
Shortages
Interrupted care
Poisoning
ER visits
Emergency departments documented dilution-related toxicity and clinicians warned that missed vaccinations and delayed chronic care compounded population-level risk, particularly among vulnerable and uninsured groups.
The fallout extended beyond individual harm: clinics diverted attention from chronic disease management, pharmacies faced 'Drive-Thru' chaos and inventory audits, and prescribers wrestled with red flags on questionable Script - Prescription requests. Rebuilding trust requires clear guidelines, stronger surveillance, accessible care, and proactive communication to prevent future waves of harm.
Building Resilience: Combating Myths with Transparent Communication
Communities tired of mixed messages respond to honesty and clarity. Narratives that respect fears, not dismiss them, rebuild trust. Trusted spokespeople outline clear steps for families.
Clinicians should share evidence and uncertainty openly, explain trials and limits, and avoid overselling single studies or anecdotes.
Pharmacies and frontline staff can help by labeling risks, offering Meds Check conversations, and flagging red flags when demand spikes.
Combining accessible data, patient stories, and rapid corrections of errors creates durable defenses against rumors and reduces harms fast. Rapid feedback mechanisms keep corrections visible everywhere.